
EMPIRICAL PROOF THAT HEALTHCARE COLLABORATION PLATFORMS ENGAGE USERS
A 2016 market report from Gartner Research claims: “Clinical communication and collaboration platforms can improve care quality, care team effectiveness and the patient experience.” but there has been no data proving that users would engage in such platforms, until now.

When we set out to build Vela, we wanted to bring the collaborative values of platforms like Slack to healthcare. More specifically we wanted to enable care teams to collaborate with patients and their caregivers much more easily and conveniently than by telephone.
The big question is always: will users engage in a new platform? Teams of co-workers in business engage in collaboration platforms but healthcare is more challenging. Lack of engagement is the bête noire of healthcare applications purposed for patients. Take so-called “patient portals”, for example — these have had low levels of user engagement by patients.
By “engagement” in this context, we cannot mean logins-per-day. This isn’t Facebook. The point of healthcare collaboration is to engage patients and their caregivers during incidents that require attention, these can be episodic or ongoing. We know that patients and their families are often fully engaged in times of health crisis, the question is: would they engage in an online platform if healthcare resources were made available there? Or would they rely solely on in-person and telephone communication?
By “engagement” in this context, we cannot mean logins-per-day. This isn’t Facebook.
It’s important to note that these resources, often nurses and social workers by training who are referred to as ‘care managers’, are provided by health insurers and hospitals to mitigate risks for patients that are regarded as “high risk”. It makes financial sense to make such resources available to reduce unnecessary costs (eg. emergency room visits). Insurers understand the actuarial trends for high risk patients, who make up a disproportionate percentage of overall health costs.
We can crystallize engagement in health care collaboration platforms along two critical dimensions:
a) Incidents — At times of incidents, do patients and/or their caregivers reach out to care teams online?
b) Patient risk — Do patients with higher health risks, and their care teams, use collaboration platforms more than those with lower risks?
If the answer to either of these questions was no, this would mean the collaboration platform was not engaging users when they needed it, which is the point!

The conversation around incidents
We analyzed data for a patient population (1000 users) who were part of a care management program that included collaborative software and at least one care manager making up their care team. Often times a care team was comprised of a nurse and a social worker, and many patients had family members in their care team. This patient population incurred incidents (hospitalizations) so we were able to analyze the collaborative conversation before and after each incident.
What we want to understand is: how does the nature of the collaborative care team conversation change following an incident? If patients and their care teams truly engage in such a platform then the data should show a material change when a hospitalization occurs.
For all that is and will be invested in healthcare collaboration, this is the quintessential question.
The investment in licensing a collaboration platform is just the beginning. An organization must commit to training, onboarding, supporting and investing in the change management to get healthcare professionals to use the solution. It’s crucial to understand if users will engage in it!
The data shows that patients and their care teams do engage in online collaboration when a hospitalization incident occurs. A sample size of ~2k patients with a care team communicating online, across ~1.5k incidents over an 18 month period. The classification of messaging following an incident shifted to be more empathetic, more clinical, and also that the volume of communication increased significantly (38%) in the week following the incident.
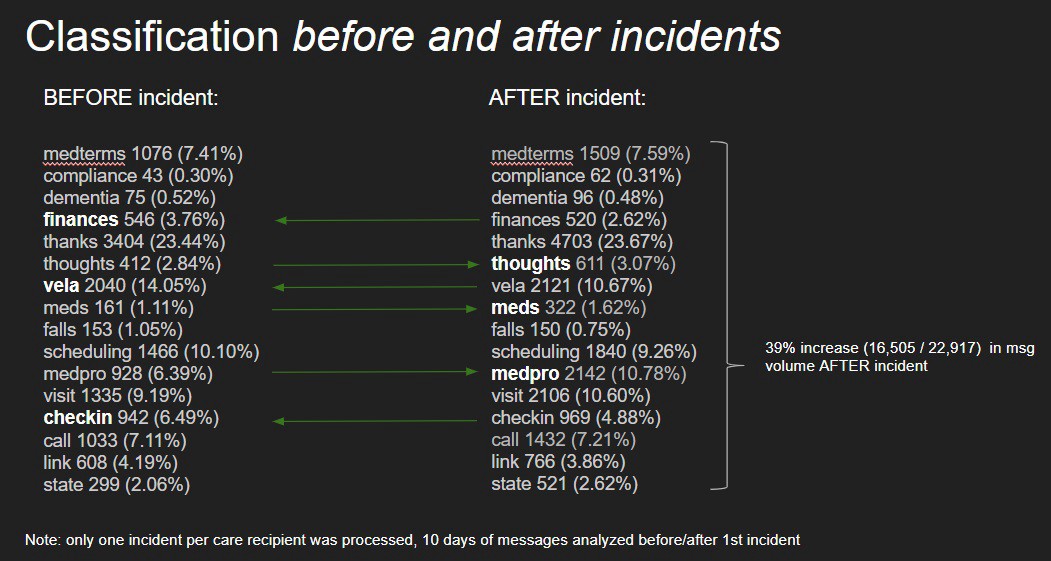
The analysis shows that the week following a hospitalization, the patient’s caregiver and care team used terms that were more empathetic (class: ‘thoughts’), more clinical (class: ‘meds’, class: ‘medical professional’). This means they were using more expressions like: “how mom is doing ok”, “what meds did they prescribe?”, “what did the doctor tell you?”.
The increase in volume is an essential finding as this proves that when an incident happens care team engage far more in online collaboration. A lot of questions get answered here, such as “is a sore throat a side-effect of this new medication?” or “can he eat the morning of the checkup next Thursday?” or “he’s doing a bit better this morning, thank you”.
Not only is there value in getting answers to questions and providing status updates but there is the positive psychological impact of knowing a care team is taking care of you. Yes this can be done by live phone calls but it’s much easier to communicate online asynchronously (each person responding when they have the chance), and many things that cannot be sent by phone (a picture, a short video, a link, an instruction guide, etc.)
Following a hospitalization, patients and their care team engage and collaborate more online.

Collaboration and patient risk
Next we analyzed online collaboration across patient risk profiles. Specifically we looked at diagnoses from MDS data for elderly patients and cross-correlated this with messaging frequency among the care teams. The data was analyzed from ~3.5k patients active on the platform over an 18month period. Care teams included at least one healthcare professional and a family caregiver.
The data reveals that the higher the risk profile, the higher the amount of care team messaging. Patients diagnosed with arthritis, for example, represent 29% of the population analyzed, but their collaborative messaging corresponds to levels 58% higher than those without this diagnosis.
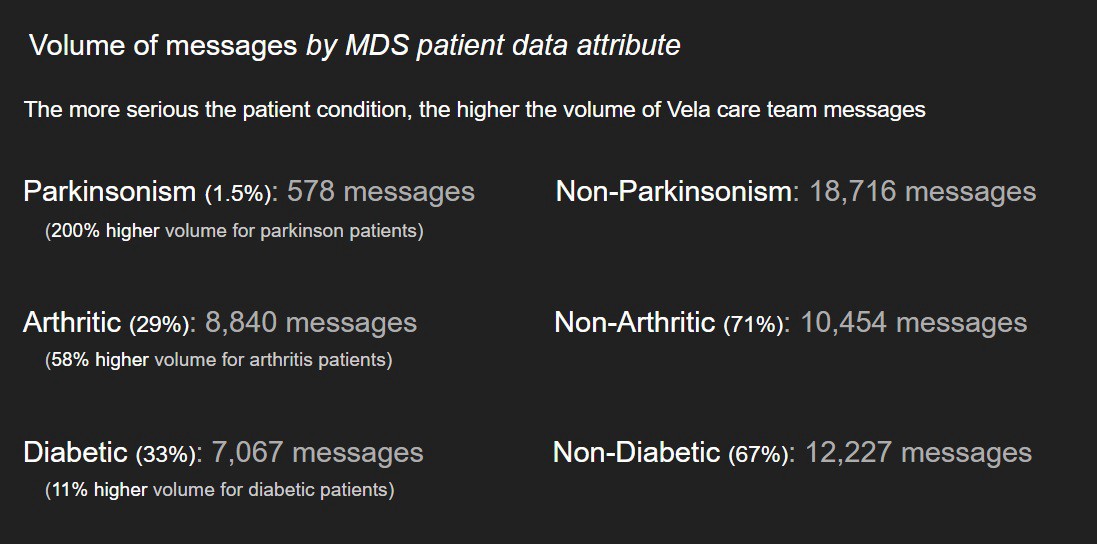
The higher the patient risk, the greater the impact of care management, and the greater the use of collaboration platforms by their care teams.
This is huge.
Care teams will engage in and leverage online collaboration platforms when collaboration is most needed. This engagement is not about low-risk or relatively healthy patients, it’s about high-risk patients. This is precisely where healthcare organizations are focused. Rhode Island Primary Care Physician’s organization (RIPCPC) recently provided a testimonial for Vela. Noah Benedict, their Chief Operating Officer, stated that their highest risk patients and their care team collaborating online improved outcomes and reduced costs. Online collaboration eliminated phone-tag, a 95% response rate to patient messages. Reaching more patients with the same resources.
The data proves that healthcare collaboration platforms are engaging when it matters most: with high-risk patients and following incidents.

The collaborative transformation that ‘unicorn’ platforms such as Slack have brought to business is happening in healthcare, with high-risk patient populations, and the impact is substantial!
More insights like this:
-

7 Immune System Booster Tips for Seniors
Read more: 7 Immune System Booster Tips for SeniorsThe immune system is the body’s first line of defense against viruses and infections, but the aging process can weaken the immune system. Throughout the COVID-19 pandemic, this became an increased concern for the caregivers of older or immunocompromised adults, as the risk of more severe symptoms and outcomes was much higher in these…
-

Massachusetts Adult Foster Care Eligibility Defined
Read more: Massachusetts Adult Foster Care Eligibility DefinedFor family caregivers, it’s crucial to create a community of support and utilize all the programs and resources available to you to improve your caregiver experience. In Massachusetts, the Adult Foster Care Program can be an excellent source of support, but eligibility can sometimes be overwhelming to navigate on your own. “The Massachusetts Adult Foster…
